 Dr. Chris Armstrong, the Director of OMF’s Melbourne ME/CFS Collaboration, and his team recently published a paper on their work looking at which genes were most impactful to metabolites in ME/CFS and which were most impactful in controls.
Dr. Chris Armstrong, the Director of OMF’s Melbourne ME/CFS Collaboration, and his team recently published a paper on their work looking at which genes were most impactful to metabolites in ME/CFS and which were most impactful in controls.
When comparing the genes identified between the two groups, two related to cortisol production were found to be impactful in ME/CFS and not in controls. This suggests that the cortisol and stress pathway might have a bigger impact on metabolism in ME/CFS than controls, and that may be because of increased sensitivity to cortisol or increased cortisol production.
Want to hear more about this publication?
If you want to dive deeper into this paper, join Dr. Danielle Meadows, OMF’s VP of Research Programs, for the first ever OMF Journal Club on December 17 at 4pm ET. During the session, Dr. Meadows will talk through the main ideas of the paper, the figures, and the implications for people with ME/CFS and Long COVID. If you’re not able to join the session live, a recording will be sent to all registrants.
The Bigger Picture
Put simply, genetic variants can impact metabolite levels, which can alter various pathways and lead to a disease or clinical phenotype. In general, genetic studies try to understand genetic variants that are associated with a change in the body. More specifically, this paper describes a metabolite genome-wide association study (mGWAS), which differs from a general GWAS. The graphic below gives a high-level view of how mGWAS relates to general GWAS.
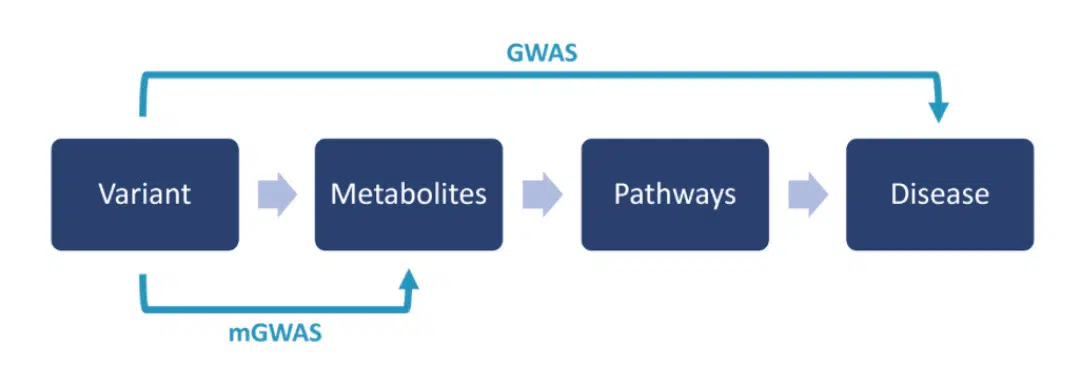
GWAS tries to find genetic variants that are associated with a disease, and mGWAS tries to find genetic variants that are associated with metabolite levels—explaining how a genetic variant might lead to a disease via altered metabolism. Given the relationship between GWAS and mGWAS, this paper provides complementary information to some of the recent publications on genetic contributions to ME/CFS.
This paper is part of the Biological Outlier and Subtyping Software for ME/CFS project. Read the full paper in iScience.